What Is Guillain-Barré Syndrome?
In Guillain-Barré syndrome (GBS), the body’s immune system attacks the nerves and its lining. This causes temporary weakness or even paralysis (being unable to move) in parts of the body.
GBS is rare, but can be serious. If it affects the chest muscles, for example, a person can have breathing trouble and need to use a ventilator for a while. The good news is that the condition is treatable and most children make a full recovery.
What happens in GBS ?
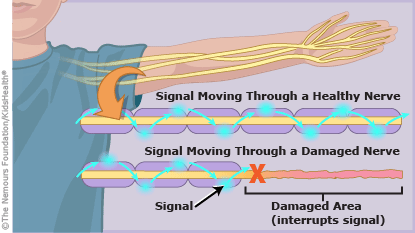
The peripheral nerves send signals from the brain to the muscles and tell them to move. They also send sensory signals (such as touch, pressure, temperature, and pain) to the brain.
Guillain-Barré syndrome temporarily damages the the nerves and its coating, which interrupts the signals. So someone with the condition may have weakness or problems moving, or may feel pain, numbness, or tingling in the arms or legs.
What causes GBS?
Many children with GBS have had a viral or bacterial infection in the 2 weeks before symptoms began. The infections usually are in the respiratory system or gastrointestinal tract. These infections trigger the immune system to produce proteins called antibodies. Normally the antibodies help destroy invading bacteria or viruses. But in GBS, these antibodies mistakenly damage parts of the peripheral nerves and its coating.
What are the symptoms of GBS?
Symptoms of GBS, in the order that they usually happen, include:
- tingling or pain in the toes and fingertips
- weakness or pain in the legs that causes trouble walking, this can then progress to involve hands and arms
- loss of reflexes (for example, the knee doesn’t jerk when it’s tapped)
- facial weakness
- inability to move the eye in some cases
- breathing problems
How is GBS diagnosed?
Doctors ask questions about the symptoms and do an exam. If GBS seems likely, the doctor clinically suspects a diagnosis of GBS and start treatment. They also might order tests to support the diagnosis, such as:
- a spinal tap (lumbar puncture) to check for cells and chemicals in the spinal fluid
- nerve conduction velocity (NCV) test to see how fast electrical signals move through a nerve
- MRI to look inside the brain and spinal cord
Sometimes these tests may be normal when done early, hence it is important that the management of GBS is clinically driven once the doctor suspects it.
How is GBS treated?
Treatments that can speed recovery include:
- Immunoglobulin (IVIg) therapy: This injection of healthy antibodies helps lessen the immune system’s attack on the body.
And/Or - Plasmapheresis or plasma exchange (PLEX): A machine pumps blood out of the body, removes the cells producing the antibodies and the antibodies attacking the nervous system, and returns blood to the body.
Most children with the condition usually get medicines to ease nerve related pain (gabapentin/pregabalin/ amitryptiline) and to prevent blood clots (stockings/blood thinner injections) if they can’t move their legs easily.
Most children with GBS get care in a hospital so doctors and nurses can check how they’re doing. Sometimes they’re cared for in an intensive care unit (ICU). This lets doctors and nurses regularly check on vital signs, such as blood pressure and heart rate, and pay close attention to how the body is doing. Some children need brief period of ventilation and a nasogastric tube to support their feeding.
How long a child stays in the hospital depends on how serious the symptoms are. Some children are in the hospital for only a few days, while others stay for several weeks.
Even after coming home from the hospital, children might need some time before feeling better. Some children with GBS might use a wheelchair or a walker until they regain their strength. Most will need physiotherapy to get their bodies moving well again.